In the "high-sensitivity cardiac troponin era," will the role of cardiac imaging in the ED change?
As high-sensitivity cardiac troponin (hs-cTn) assays become more and more common, cardiac imaging becomes less necessary for ruling out acute myocardial infarction (AMI) in ED patients with acute chest pain, but might be useful to prevent unnecessary or aggressive treatments write experts in July's volume of the American Heart Journal.
ACVP blog has covered the groundbreaking research on the high-sensitivity cardiac troponin tests since early last year, when we reported a new strategy that could rule out acute myocardial infarction within one hour, and rule it in with 75 percent accuracy. In June, two studies publishes in JAMA Cardiology lent further support to one-hour algorithms.
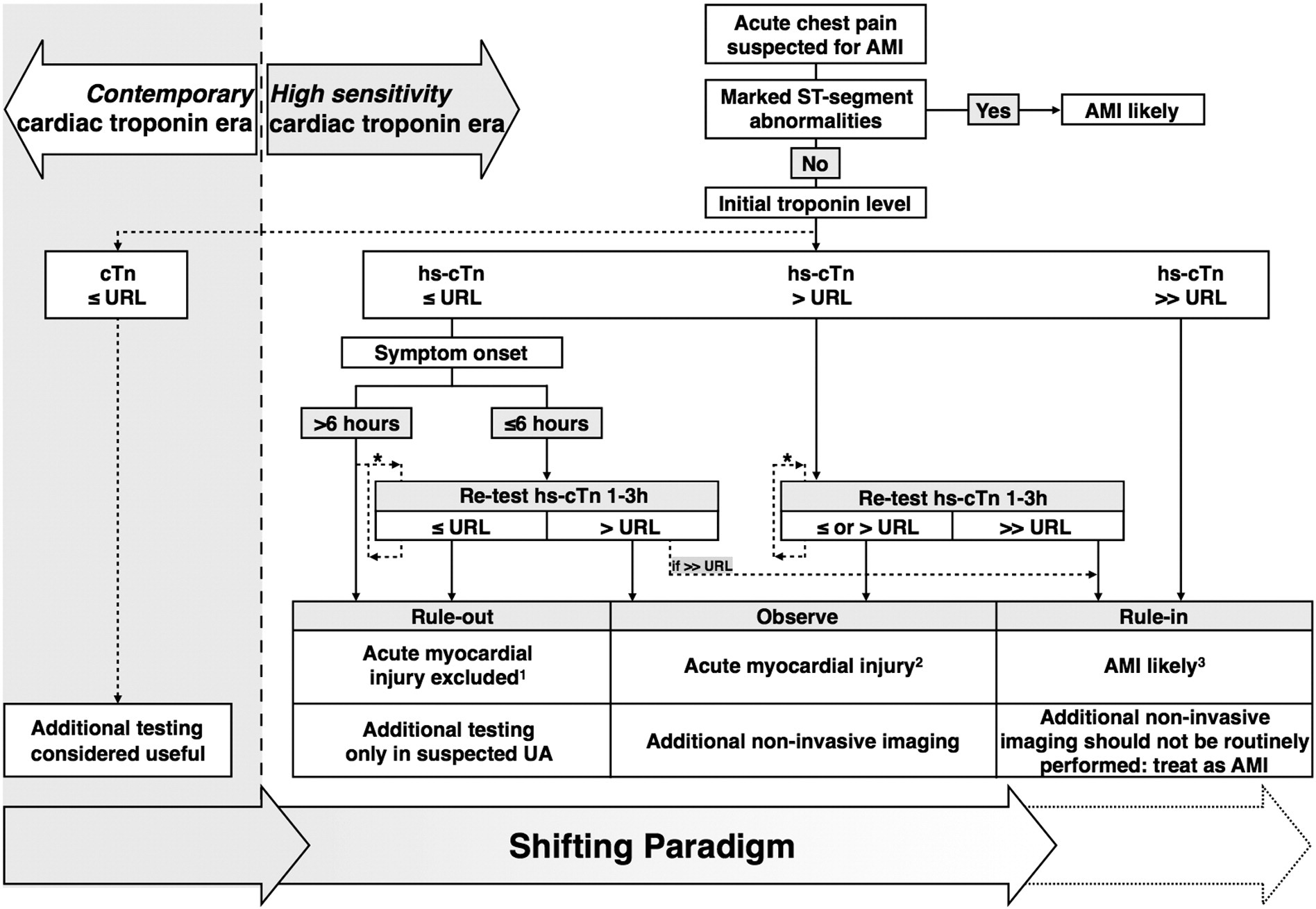
The speed and safe, accurate "rule out" of acute myocardial infarction through these cardiac biomarker tests "challenges [the] need" for noninvasive imaging prior to patient discharge when troponin values are normal, write the authors of the American Heart Journal article.
In fact, in patients with hs-cTn levels less than or equal to the 99th percentile upper reference limit, or at undetectable levels, AMI "can be ruled out confidently (ie, prognosis is excellent and the rate of missing AMI is extremely low)"—so confidently that additional testing is "generally discouraged to prevent false-positive test results," write the authors.
Cardiac imaging as the gatekeeper to aggressive therapy?
Instead, noninvasive cardiac imaging in these ED applications might shift toward "characterizing myocardial disease when hs-cTn values are (mildly) abnormal," write the authors.
Why? "Defining the upper hs-cTn cutoff values to diagnose AMI is more gradual and less absolute," write the authors. "The increased diagnostic sensitivity of hs-cTn assays comes at the expense of a lower specificity and positive predicitive value to diagnose AMI."
However, for particularly high hs-cTn levels, AMI is so likely that only routine, indicated echocardiography should be conducted so as to "not unnecessarily delay invasive management," write the authors.
So where does the bulk of cardiac imaging fit in? "The challenge now lies in the clinical interpretation of mildly abnormal hs-cTn levels," write the authors.
"Mildly abnormal hs-cTn levels" are above the upper reference limit but not so high that there is a high likelihood of AMI. "This may reflect AMI or acute noncoronary (structural) myocardial disease, or may be associated with chronic stable CAD, renal dysfunction, or even be a variation of normal (in the elderly and men)," write the authors.
The goal? Not subjecting patients without AMI to "unnecessary aggressive antithrombotic, antiplatelet therapy, or invasive coronary angiography," write the authors. Noninvasive cardiovascular imaging could "serve as a gatekeeper."
For the authors' views on specific tests, read from "In patients with mildly abnormal hs-cTn levels."
Work still needs to be done, however, to define the "most appropriate imaging modality or even multicomponent strategy," write the authors in their conclusion. "An individualized approach of 'tailored diagnostics' seems plausible."
What do you think? What are you seeing at your practice? Has the paradigm shifted from rule-out to rule-in? Leave a comment!