NSTEMI: Early Hospital Care
Standard Medical Therapies
Oxygen
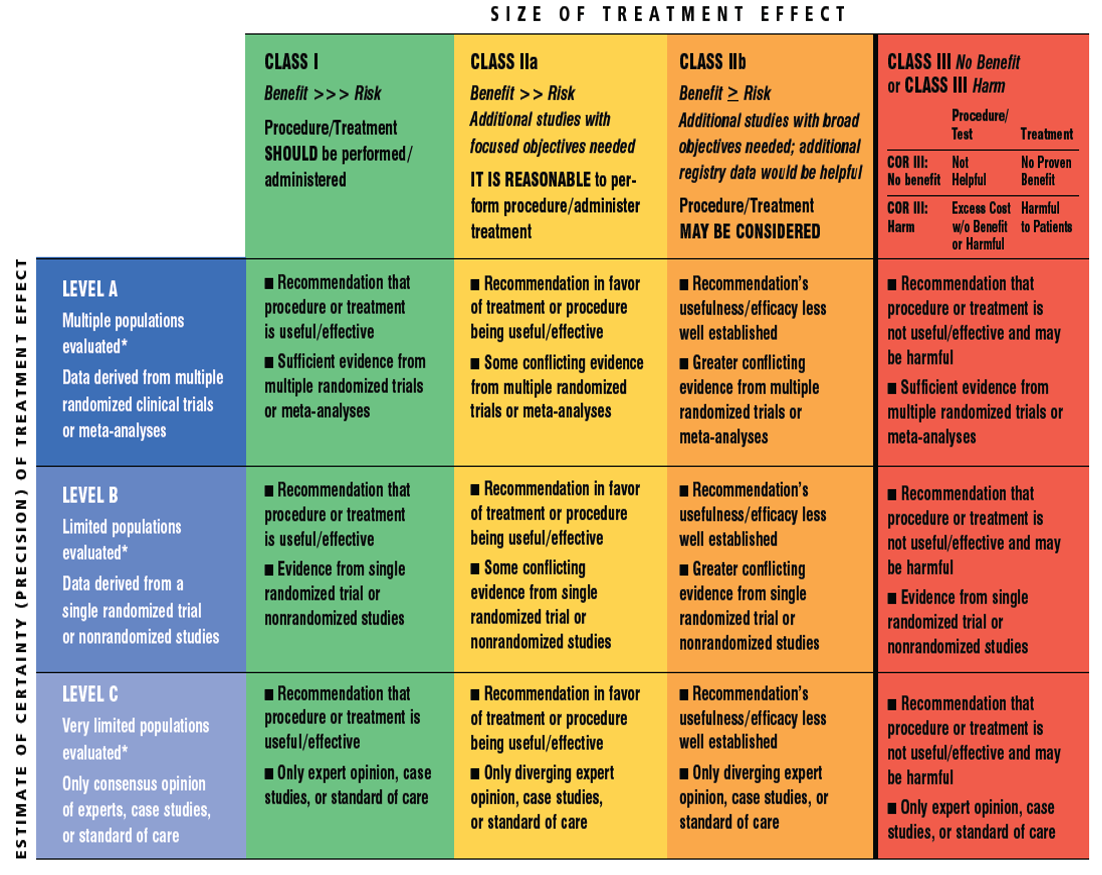
| Recommendation | Class | Level |
| Supplemental oxygen should be administered to patients with NSTE-ACS with arterial oxygen saturation less than 90%, respiratory distress, or other high-risk features of hypoxemia. | I | C |
Analgesic Therapy
| Recommendation | Class | Level |
| In the absence of contraindications, it may be reasonable to administer morphine sulfate intravenously to patients with NSTE-ACS if there is continued ischemic chest pain despite treatment with maximally tolerated anti-ischemic medications. | IIb | B |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) (except aspirin) should not be initiated and should be discontinued during hospitalization for NSTE-ACS because of the increased risk of MACE associated with their use. | III | B |
Beta-Adrenergic Blockers
| Recommendation | Class | Level |
| Oral beta-blocker therapy should be initiated within the first 24 hours in patients who do not have any of the following: 1) signs of HF, 2) evidence of low-output state, 3) increased risk for cardiogenic shock, or 4) other contraindications to beta blockade (e.g., PR interval >0.24 second, second- or third-degree heart block without a cardiac pacemaker, active asthma, or reactive airway disease). | I | A |
| In patients with concomitant NSTE-ACS, stabilized HF, and reduced systolic function, it is recommended to continue beta-blocker therapy with 1 of the 3 drugs proven to reduce mortality in patients with HF: sustained-release metoprolol succinate, carvedilol, or bisoprolol. | I | C |
| Patients with documented contraindications to beta blockers in the first 24 hours of NSTE-ACS should be re-evaluated to determine their subsequent eligibility. | I | C |
| It is reasonable to continue beta-blocker therapy in patients with normal LV function with NSTE-ACS. | IIa | C |
| Administration of intravenous beta blockers is potentially harmful in patients with NSTE-ACS who have risk factors for shock. | III | B |
Calcium Channel Blockers
| Recommendation | Class | Level |
| In patients with NSTE-ACS, continuing or frequently recurring ischemia, and a contraindication to beta blockers, a nondihydropyridine calcium channel blocker (CCB) (e.g., verapamil or diltiazem) should be given as initial therapy in the absence of clinically significant LV dysfunction, increased risk for cardiogenic shock, PR interval greater than 0.24 second, or second- or third-degree atrioventricular block without a cardiac pacemaker. | I | B |
| Oral nondihydropyridine calcium antagonists are recommended in patients with NSTE-ACS who have recurrent ischemia in the absence of contraindications, after appropriate use of beta blockers and nitrates. | I | C |
| CCBs are recommended for ischemic symptoms when beta blockers are not successful, are contraindicated, or cause unacceptable side effects. | I | C |
| Long-acting CCBs and nitrates are recommended in patients with coronary artery spasm. | I | C |
| Immediate-release nifedipine should not be administered to patients with NSTE-ACS in the absence of beta-blocker therapy. | III | B |
Cholesterol Management
| Recommendation | Class | Level |
| High-intensity statin therapy should be initiated or continued in all patients with NSTE-ACS and no contraindications to its use. | I | A |
| It is reasonable to obtain a fasting lipid profile in patients with NSTE-ACS, preferably within 24 hours of presentation. | IIa | C |
Inhibitors of Renin-Angiotensin-Aldosterone System
| Recommendation | Class | Level |
| ACE inhibitors should be started and continued indefinitely in all patients with LVEF less than 0.40 and in those with hypertension, diabetes mellitus, or stable CKD (Section 7.6), unless contraindicated. | I | A |
| ARBs are recommended in patients with HF or MI with LVEF less than 0.40 who are ACE inhibitor intolerant. | I | A |
| Aldosterone blockade is recommended in patients post–MI without significant renal dysfunction (creatinine >2.5 mg/dL in men or >2.0 mg/dL in women) or hyperkalemia (K >5.0 mEq/L) who are receiving therapeutic doses of ACE inhibitor and beta blocker and have a LVEF 0.40 or less, diabetes mellitus, or HF. | I | A |
| ARBs are reasonable in other patients with cardiac or other vascular disease who are ACE inhibitor intolerant. | IIa | B |
| ACE inhibitors may be reasonable in all other patients with cardiac or other vascular disease. | IIb | B |
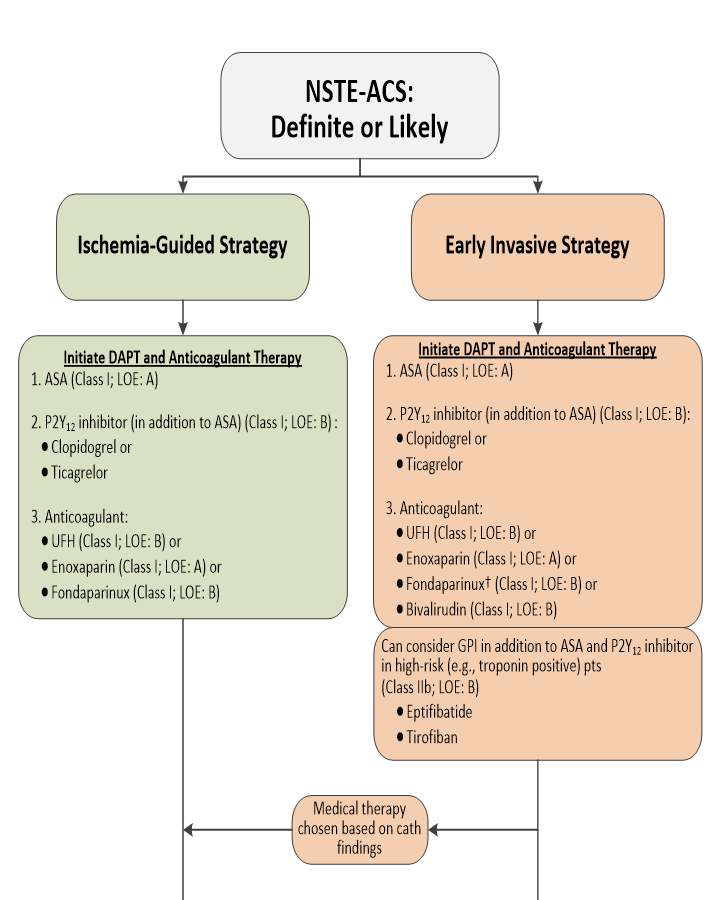
Algorithm for Management of Patients With Definite or Likely NSTE-ACS
Factors Associated With Appropriate Selection of Early Invasive Strategy or Ischemia-Guided Strategy in Patients With NSTE-ACS
| Immediate invasive (within 2 h) | Refractory angina |
| Signs or symptoms of HF or new or worsening mitral regurgitation | |
| Hemodynamic instability | |
| Recurrent angina or ischemia at rest or with low-level activities despite intensive medical therapy | |
| Sustained VT or VF | |
| Ischemia-guided strategy | Low-risk score (e.g., TIMI [0 or 1], GRACE [<109]) |
| Low-risk Tn-negative female patients | |
| Patient or clinician preference in the absence of high-risk features | |
| Early invasive (within 24 h) | None of the above, but GRACE risk score >140 |
| Temporal change in Tn (Section 3.4) | |
| New or presumably new ST depression | |
| Delayed invasive (within 25-72 h) | None of the above but diabetes mellitus |
| Renal insufficiency (GFR <60 mL/min/1.73 m²) | |
| Reduced LV systolic function (EF <0.40) | |
| Early postinfarction angina | |
| PCI within 6 mo | |
| Prior CABG | |
| GRACE risk score 109–140; TIMI score ≥2 |
Initial Oral and Intravenous Antiplatelet Therapy in Patients With Definite or Likely NSTE-ACS Treated With an Initial Invasive or Ischemia-Guided Strategy
| Recommendation | Class | Level |
| Non–enteric-coated, chewable aspirin (162 mg to 325 mg) should be given to all patients with NSTE-ACS without contraindications as soon as possible after presentation, and a maintenance dose of aspirin (81 mg/d to 162 mg/d) should be continued indefinitely. | I | A |
| In patients with NSTE-ACS who are unable to take aspirin because of hypersensitivity or major gastrointestinal intolerance, a loading dose of clopidogrel followed by a daily maintenance dose should be administered. | I | B |
| A P2Y12 inhibitor (either clopidogrel or ticagrelor) in addition to aspirin should be administered for up to 12 months to all patients with NSTE-ACS without contraindications who are treated with either an early invasive or ischemia-guided strategy. Options include: •Clopidogrel: 300-mg or 600-mg loading dose, then 75 mg daily •Ticagrelor: 180-mg loading dose, then 90 mg twice daily | I | B |
| It is reasonable to use ticagrelor in preference to clopidogrel for P2Y12 treatment in patients with NSTE-ACS who undergo an early invasive or ischemia-guided strategy. | IIa | B |
| In patients with NSTE-ACS treated with an early invasive strategy and dual antiplatelet therapy (DAPT) with intermediate/high-risk features (e.g., positive troponin), a GP IIb/IIIa inhibitor may be considered as part of initial antiplatelet therapy. Preferred options are eptifibatide or tirofiban. | IIb | B |
Initial Parenteral Anticoagulant Therapy in Patients With Definite NSTE-ACS
| Recommendation | Class | Level |
| In patients with NSTE-ACS, anticoagulation, in addition to antiplatelet therapy, is recommended for all patients irrespective of initial treatment strategy. Treatment options include: •Enoxaparin: 1 mg/kg subcutaneous (SC) every 12 hours (reduce dose to 1 mg/kg SC once daily in patients with creatinine clearance [CrCl] <30 mL/min), continued for the duration of hospitalization or until PCI is performed. An initial intravenous loading dose is 30 mg. | I | A |
| •Bivalirudin: 0.10 mg/kg loading dose followed by 0.25 mg/kg per hour (only in patients managed with an early invasive strategy), continued until diagnostic angiography or PCI, with only provisional use of GP IIb/IIIa inhibitor, provided the patient is also treated with DAPT. •Fondaparinux: 2.5 mg SC daily, continued for the duration of hospitalization or until PCI is performed. | I | B |
| •If PCI is performed while the patient is on fondaparinux, an additional anticoagulant with anti-IIa activity (either UFH or bivalirudin) should be administered because of the risk of catheter thrombosis. •UFH IV: initial loading dose of 60 IU/kg (maximum 4,000 IU) with initial infusion of 12 IU/kg per hour (maximum 1,000 IU/h) adjusted per activated partial thromboplastin time to maintain therapeutic anticoagulation according to the specific hospital protocol, continued for 48 hours or until PCI is performed. | I | B |
| In patients with NSTE-ACS (i.e., without ST elevation, true posterior MI, or left bundle-branch block not known to be old), intravenous fibrinolytic therapy should not be used. | III | A |
Early Invasive and Ischemia: Guided Strategies
| Recommendation | Class | Level |
| An urgent/immediate invasive strategy (diagnostic angiography with intent to perform revascularization if appropriate based on coronary anatomy) is indicated in patients (men and women) with NSTE-ACS who have refractory angina or hemodynamic or electrical instability (without serious comorbidities or contraindications to such procedures). | I | A |
| An early invasive strategy (diagnostic angiography with intent to perform revascularization if appropriate based on coronary anatomy) is indicated in initially stabilized patients with NSTE-ACS (without serious comorbidities or contraindications to such procedures) who have an elevated risk for clinical events. | I | B |
| It is reasonable to choose an early invasive strategy (within 24 hours of admission) over a delayed invasive strategy (within 25 to 72 hours) for initially stabilized high-risk patients with NSTE-ACS. For those not at high/intermediate risk, a delayed invasive approach is reasonable. | IIa | B |
| In initially stabilized patients, an ischemia-guided strategy may be considered for patients with NSTE-ACS (without serious comorbidities or contraindications to this approach) who have an elevated risk for clinical events. | IIb | B |
| The decision to implement an ischemia-guided strategy in initially stabilized patients (without serious comorbidities or contraindications to this approach) may be reasonable after considering clinician and patient preference. | IIb | C |
| An early invasive strategy (i.e., diagnostic angiography with intent to perform revascularization) is not recommended in patients with: • Extensive comorbidities (e.g., hepatic, renal, pulmonary failure, cancer), in whom the risks of revascularization and comorbid conditions are likely to outweigh the benefits of revascularization. • Acute chest pain and a low likelihood of ACS • Who are troponin-negative, especially women. | III | C |

